Ulcerative Colitis and How Acupuncture & Chinese Herbal Medicine Can Help
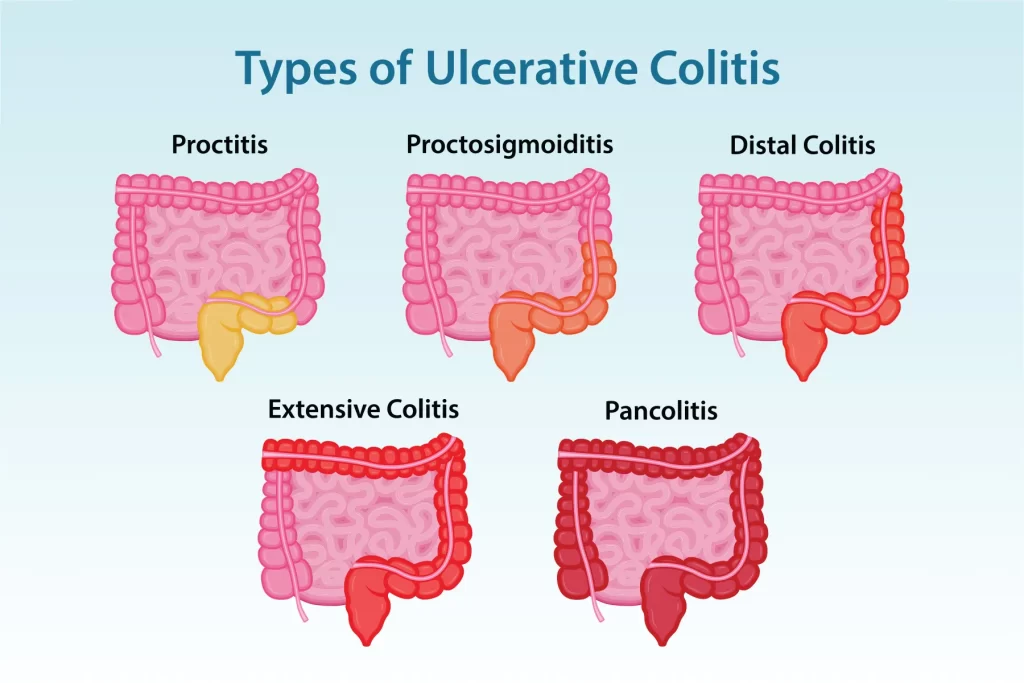
Ulcerative colitis (UC) causes inflammation and ulceration of the colon lining and commonly leads to abdominal pain, urgency, bloody diarrhoea and fatigue. Conventional treatments (5-ASA, steroids, immunomodulators, biologics) are effective for many people but aren’t a universal solution, side effects, incomplete response, and relapses are common. Over the last two decades researchers have explored complementary approaches, and acupuncture plus Traditional Chinese Medicine (TCM) herbal formulas are among the most-studied. Below I summarise the best available evidence, proposed mechanisms, safety considerations, and practical suggestions for patients considering integrative care.
What the clinical studies show
Acupuncture — Randomized trials and systematic reviews show that acupuncture (often used with moxibustion or alongside drugs) can improve clinical symptoms, overall “effective rate,” and some patient-reported outcomes in UC compared with drug therapy alone in several trials. The pooled data are promising but heterogeneous and many trials are small or use different outcome measures, so more high-quality sham-controlled trials are still needed. (BioMed Central)
Chinese herbal medicine (CHM) — Multiple randomized controlled trials and recent systematic reviews/meta-analyses report that certain herbal formulas (and combinations such as curcumin + QingDai) can increase clinical response and remission rates, and may be non-inferior to mesalazine in some studies. Systematic reviews find encouraging signals but note variability in study quality and the need for larger, well-designed RCTs. (MDPI)
Key study highlights
A comprehensive systematic review of acupuncture trials for UC pooled randomized controlled trials and found improved overall effectiveness when acupuncture was added to conventional therapy, but the authors emphasised methodological limits and called for better-designed sham-controlled trials. (BioMed Central)
A recent systematic review and meta-analysis of herbal medicines for active UC synthesized randomized trials and concluded herbal treatments can improve clinical outcomes (response/remission/endoscopic outcomes) in some trials — again with heterogeneity between studies and variable quality. (MDPI)
Specific modern formulations are now being tested in rigorous trials. For example, randomized controlled trials have compared Fufangkushen capsules and other standardized formulas to mesalazine and reported comparable benefit in certain endpoints, while newer compounds (e.g., CDD-2103) have progressed to controlled clinical trials. These larger, better-designed studies are important steps toward clearer recommendations. (Wiley Online Library)
Combination approaches have also shown benefit: trials of curcumin + QingDai for active UC have reported significant improvements in clinical endpoints compared with control groups in recent clinical evaluations. (CGH Journal)
How might acupuncture and herbs work?
Research suggests several plausible mechanisms:
Immune modulation: acupuncture and certain herbs appear to reduce pro-inflammatory cytokines and regulate immune cell activity relevant to UC.
Mucosal protection & healing: some herbal compounds may promote mucosal repair and reduce oxidative stress in the gut lining.
Gut microbiome: acupuncture and herbal treatments have been associated with changes in microbiota composition that—at least in animal studies—correlate with reduced inflammation.
Symptom control and quality of life: acupuncture can reduce visceral pain, improve bowel function and lower anxiety/depression symptoms that commonly worsen UC quality of life. Mechanistic reviews and preclinical studies support these pathways, but human mechanistic data remain limited. (OUP Academic)
Safety and interactions — what to watch for
Herbal-drug interactions: some herbs interact with conventional drugs (e.g., affecting metabolism). Always tell your gastroenterologist and pharmacist about any herbs you take.
Quality control: herbal products vary in purity and dose. Prefer standardized extracts or products studied in clinical trials, and use reputable suppliers.
Acupuncture safety: when performed by a registered practitioner using single-use sterile needles, acupuncture is generally safe. Minor side effects (bruising, soreness) are most common; major complications are rare.
Do not stop prescribed medicine without advice: integrative approaches are usually used with conventional therapy, not as an abrupt replacement.
Practical, evidence-based approach for patients
Discuss with your gastroenterologist before starting herbs or acupuncture — coordinate care, especially if you’re on immunosuppressants or biologics.
Use qualified practitioners: seek a licensed acupuncturist experienced with GI/IBD patients and a TCM herbalist who understands IBD and works with your medical team.
Prefer studied formulas or standardized extracts: where possible choose formulas or products evaluated in randomized trials rather than unexplained “blends.”
Track outcomes: keep a symptom diary (frequency, bleeding, pain, urgency, energy), and ensure objective monitoring (stool calprotectin, blood tests, colonoscopy) is maintained per your gastroenterologist’s guidance.
Consider integrative trials: if suitable, participation in well-designed clinical trials helps build the evidence base and often provides close medical oversight. (BMJ Open)
Acupuncture and certain Chinese herbal medicines show encouraging results for symptom improvement and, in some trials, for clinical remission in ulcerative colitis — particularly when used alongside conventional care. Evidence is promising but heterogeneous; higher-quality, sham-controlled and multi-centre studies are needed before recommending these therapies as standalone replacements for standard medical treatments. For patients interested in integrative care: discuss it with your specialist, choose experienced practitioners, use well-characterized herbal products, and continue objective medical monitoring.
Here at Centre of Health Ivanhoe, our Physio’s and Chinese Herbalists are well trained to treat different constitutions with Ulcerative Colitis, safely and effectively.
