Acupuncture & Herbal Medicine for IBS: What the Evidence Says (and how we can help at Center of Health in Ivanhoe)
Irritable Bowel Syndrome (IBS) is common and disruptive. Recent high-quality trials suggest acupuncture can improve IBS symptoms for some people, and specific Chinese herbal medicines (including classic TCM formulas) show benefit in selected studies. At Centre of Health in Ivanhoe, we use an integrated plan (diet, stress care, acupuncture, and carefully prescribed herbs) tailored to your subtype (IBS-D, IBS-C, or IBS-M).
What is IBS—and why is it so tricky?
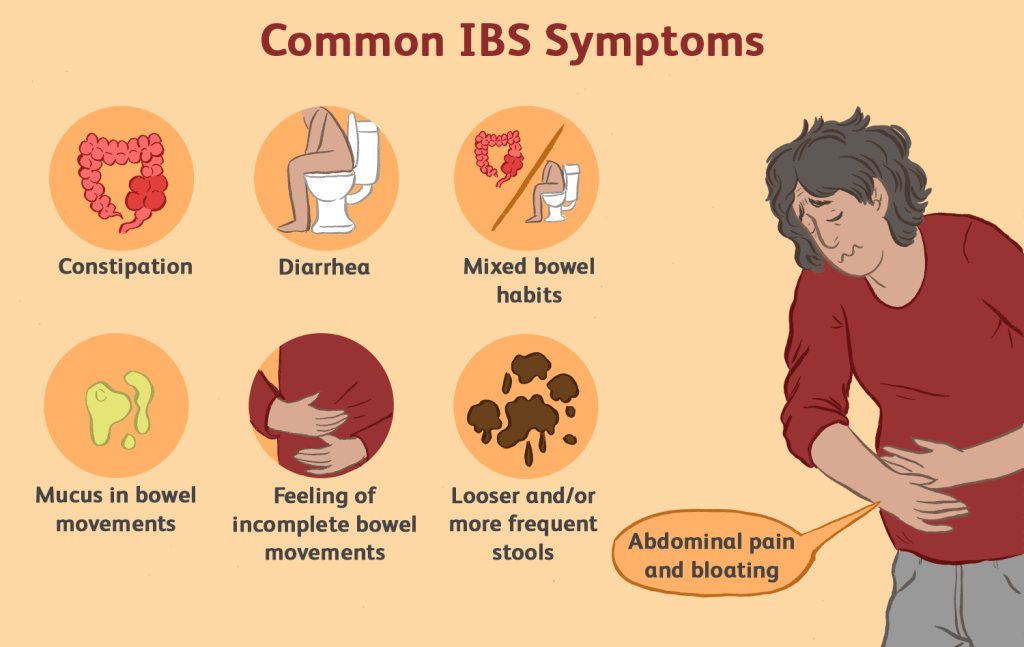
IBS is a long-term “disorder of gut–brain interaction” characterized by abdominal pain with altered bowel habits (diarrhoea, constipation, or both). It doesn’t cause structural damage, but it can seriously impact quality of life, sleep, energy, and mood. Global estimates using modern Rome criteria suggest around 4% of adults are affected at any point in time.
Conventional first-line care emphasizes a thorough medical work-up, dietary strategies (e.g., fibre and, where appropriate, a low-FODMAP approach), and targeted medicines. Some people still have persistent symptoms—this is where non-drug options like acupuncture and herbal medicine may be considered, ideally in coordination with your GP or gastroenterologist. Major guidelines remain conservative overall, but interest is growing as better trials are published.
Acupuncture for IBS: what does research show?
The newest data (2025): encouraging signals
A large multi-centre, randomized, sham-controlled trial published in Gastroenterology in 2025 (the ACTION trial) found that a 6-week course of acupuncture improved IBS symptoms (including abdominal pain and stool consistency) in adults with IBS-D, with benefits persisting beyond treatment. While not everyone responded, the trial strengthens the case that acupuncture can help some patients when carefully delivered. Gastro JournalRead by QxMDScienceDirect
Earlier results: mixed but trending positive in parts
A 2025 systematic review and meta-analysis in PLOS ONE focused on quality of life and found that acupuncture was associated with QoL improvements, though heterogeneity and risk of bias limit certainty. PLOS
Where guidelines currently land
The 2021 American College of Gastroenterology (ACG) guideline focuses on diet, peppermint oil, and gut-brain therapies; it does not make a positive recommendation for acupuncture. As newer trials (like ACTION) accumulate, recommendations may evolve—but today, acupuncture is best considered on a case-by-case basis. NICEDarmzentrum Bern
Safety
When performed by qualified practitioners using single-use sterile needles, acupuncture is generally considered safe; large prospective surveys reported mostly mild, transient adverse events (e.g., needling pain, small bruises). Serious complications are rare. BMJ+1Europe PMC
Chinese Herbal Medicine (CHM) & Peppermint Oil: what’s the evidence?
Peppermint oil (enteric-coated)
Peppermint oil has antispasmodic effects and is one of the few “herbal” options mentioned favourably in modern guidelines. A 2019 meta-analysis of randomised trials found peppermint oil superior to placebo for global IBS symptoms and abdominal pain. The ACG guideline suggests peppermint oil for overall symptom relief (conditional recommendation). Not every individual trial is positive, but taken together, evidence is reasonably supportive for many patients. BioMed CentralDarmzentrum BernThe Lancet
Practical point: enteric-coated capsules are typically used to deliver the oil to the small bowel/colon and reduce reflux/heartburn risk. Always discuss with your clinician—peppermint oil can interact with some medicines and may aggravate reflux in sensitive people. NCCIH
Classic TCM formulas (individualised by pattern)
Tongxie Yaofang (TXYF) for IBS-D: A double-blind, placebo-controlled phase II RCT (2025, BMJ Open) reported improved clinical response with TXYF granules versus placebo, with mostly mild adverse events. This is high-quality design for herbal research and adds weight to earlier protocol papers. BMJ OpenBioMed Central
Xiao Yao San (XYS): Meta-analytic work suggests potential benefit for functional GI symptoms, particularly when mood symptoms co-exist, though included trials vary in quality and standardisation. FrontiersScienceDirect
Across-formula evidence: A 2021 trial-sequential meta-analysis concluded that CHM, as a group, improved global IBS symptoms compared with placebo, with most adverse events mild; however, heterogeneity and product variability remain key caveats. A 2021 network meta-analysis comparing CHM with conventional options also suggested benefit in some outcomes, but again with variable study quality. FrontiersPLOS
Safety & quality: Herb quality, correct diagnosis (pattern differentiation), dose, and potential interactions are essential considerations. Using TGA-listed products and working with registered practitioners helps mitigate risks. Trials generally report mild adverse events, but quality control outside trials can vary—another reason to seek personalised care. Frontiers
How acupuncture might help IBS (theory meets physiology)
IBS involves altered gut motility, visceral hypersensitivity, low-grade immune activation, dysbiosis, and stress-axis changes. Acupuncture is thought to modulate the gut–brain axis, autonomic tone, and pain processing, while some CHM formulas may influence motility, serotonin pathways, bile acids, and the microbiome. These mechanisms are active research areas and help explain why some people respond while others do not. (See summary reviews and trial discussions.) gastroenterologyandhepatology.net
What treatment looks like at Centre of Health (Ivanhoe)
1) A clear plan, tailored to your subtype and goals
We start by clarifying red flags (which would warrant medical referral), your IBS subtype (IBS-D, IBS-C, or mixed), diet history, stress/sleep, and triggers. We coordinate with your GP or specialist as needed.
2) Acupuncture course
Many studies used 2–3 sessions per week over ~6 weeks; we individualise this based on your schedule and response. If you’re improving, sessions can be tapered.
3) Herbal options
For IBS-D: We may consider TXYF-based prescriptions (adapted to your pattern) or enteric-coated peppermint oil where appropriate.
For IBS-C or mixed IBS: Different classical formulas are used depending on your presentation (e.g., abdominal pain dominant, bloating dominant, or stress-linked).
We only use high-quality, TGA-listed products and check for medicine interactions.
4) Diet, stress, and sleep
We provide practical diet guidance (e.g., fibre type/amount; low-FODMAP phases in collaboration with a dietitian if needed), gentle movement, and stress-axis support (breathing work, pacing, and sleep strategies). Integrating these with acupuncture and herbs generally gives better results than any single modality.
5) Review and adjust
IBS management is iterative. We track symptoms you care about—pain days, stool form, urgency, bloating, and impact on work/life—so we can adjust quickly.
Is acupuncture or herbal medicine right for you?
May be a good fit if you:
Have persistent symptoms despite diet and standard care
Prefer non-drug options or want to reduce reliance on rescue meds
Feel stress is a major trigger and want support for the gut–brain axis
Important cautions:
New or worsening symptoms (unintentional weight loss, rectal bleeding, fever, nocturnal diarrhoea, iron-deficiency anaemia, onset after age 50) warrant medical assessment first.
Herbs can interact with medicines (e.g., anticoagulants). Always disclose your full medication/supplement list.
Book in Ivanhoe
If you’re in Ivanhoe or nearby (Heidelberg, Alphington, Kew East, Northcote), our practitioners can help you map a tailored plan that aligns with your medical care. Book an acupuncture & Chinese medicine consult at Centre of Health to get started.
